We’re letting you know that this post contains sponsored links which Your Savvy Purse receives compensation for, which may impact their order of appearance.
In the world of weight loss and diabetes management, few drugs have garnered as much attention as Ozempic. A once relatively obscure medication used to treat type 2 diabetes, Ozempic has taken the media—and the celebrity world—by storm. With reports of celebrities shedding pounds effortlessly and everyday people praising its transformative effects, it’s easy to see why Ozempic is being hailed as a “miracle” drug. But is it really the answer to our weight-loss woes, or could there be a darker side to this trend? Let’s dig into the hype, the science, and the controversies surrounding this injectable medication.
What is Ozempic?
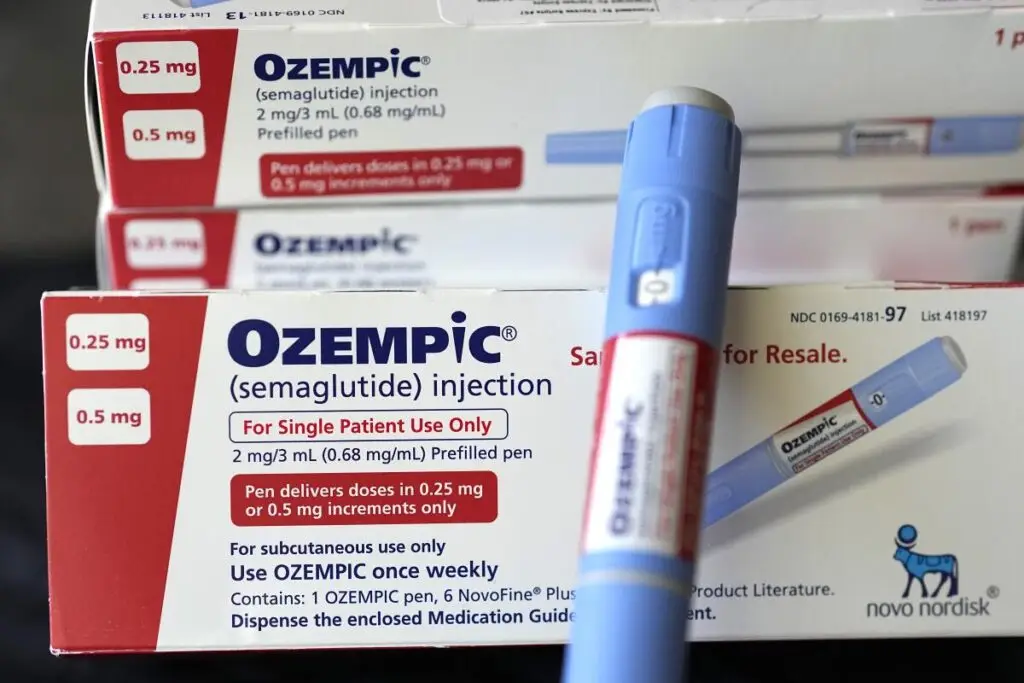
Ozempic (semaglutide) is a prescription medication developed by Novo Nordisk. It’s part of a class of drugs called GLP-1 receptor agonists, which work by mimicking a hormone that helps regulate blood sugar and appetite. Originally approved for use in patients with type 2 diabetes, Ozempic helps lower blood sugar levels by stimulating insulin release in response to meals and slowing down the emptying of the stomach. But what’s really grabbed the public’s attention is its ability to help people lose weight. In fact, the drug has recently been FDA-approved for weight management in individuals who are obese or overweight, even if they don’t have diabetes.
The “Miracle” Effect: Why Everyone Is Talking About Ozempic
If you’ve been anywhere near social media or celebrity gossip lately, you’ve probably seen someone talking about Ozempic’s weight-loss “miracle.” It’s hard to ignore the pictures of stars like Kim Kardashian and Adele, who’ve made noticeable transformations in their physiques, and have been rumored to use medications like Ozempic (though, of course, neither have confirmed it). People are reporting impressive results, often shedding tens of pounds in just a few months with minimal effort beyond taking the weekly injection.
The science behind Ozempic’s effectiveness in weight loss is real. Clinical trials have shown that the medication can reduce appetite and promote a feeling of fullness, leading to reduced calorie intake. In one major study, participants lost an average of 12-15% of their body weight over the course of 68 weeks. For those struggling with obesity, that’s a game-changer. It offers a sense of control over a condition that, for many, feels unmanageable through diet and exercise alone.
Moreover, beyond the weight loss, Ozempic has been shown to have cardiovascular benefits, like reducing the risk of heart attack and stroke in people with type 2 diabetes. These added health benefits make the medication even more enticing, especially for people already at risk for heart disease due to their weight.
The Menace: Side Effects, Accessibility, and Ethical Concerns
As with most medications, the benefits of Ozempic don’t come without potential risks—and they are raising significant concerns among healthcare professionals and users alike.
1. The Side Effects: Not All Roses
While Ozempic works wonders for many, it isn’t without its share of unpleasant side effects. The most common complaints are nausea, vomiting, diarrhea, and stomach cramps, which can be severe enough to make users question whether the benefits are worth the discomfort. These side effects tend to diminish over time, but for some, they can be a dealbreaker. More serious side effects, like pancreatitis (inflammation of the pancreas) and thyroid tumors, have been reported in some patients, though these are rare.
There’s also the risk of dehydration due to nausea and diarrhea, which can be particularly concerning for those with underlying health conditions. While the drug is considered generally safe, it’s important to remember that its side effects can make the experience of weight loss less than glamorous.
2. The Accessibility Issue: Who Gets the Drug?
One of the most glaring problems with Ozempic is its skyrocketing demand, which has led to shortages. Initially prescribed primarily for diabetes management, the drug’s newfound popularity for weight loss has caused it to be in high demand, leaving many diabetic patients struggling to access their medication. The limited availability means that those who truly need it for managing their blood sugar levels could be forced to go without, which poses a significant public health issue.
In addition, Ozempic comes with a hefty price tag, often ranging from $900 to $1,200 per month without insurance. This can make it an unfeasible option for many people, especially those who are simply looking to lose weight. While some insurance plans cover Ozempic for weight loss, the cost still remains a barrier for millions, which brings us to the ethical debate surrounding the drug’s use.
3. Ethical Concerns: Weight Loss or Weight Obsession?
The use of Ozempic for weight loss raises a broader ethical conversation. Many experts are concerned about the long-term implications of using a drug to achieve weight loss, especially given society’s increasing obsession with thinness. Is it responsible to promote a medication that might become a shortcut to weight loss without addressing the deeper issues of nutrition, exercise, and mental health?
Additionally, the rapid rise in non-diabetic individuals using Ozempic for aesthetic reasons could lead to further body image pressures. With weight-loss drugs now more accessible than ever, could we be pushing an unhealthy “quick fix” mentality rather than encouraging sustainable, holistic approaches to health and well-being?
Is Ozempic a Miracle or a Menace?
At the end of the day, whether Ozempic is a miracle or a menace depends on your perspective. For those struggling with obesity or type 2 diabetes, Ozempic is undoubtedly a medical breakthrough that can change lives—helping individuals control their blood sugar, lose weight, and reduce the risk of cardiovascular disease. For them, it may truly feel like a miracle.
However, for others, the overuse of the drug for weight loss—combined with the uncomfortable side effects, the high cost, and the potential for ethical concerns—means it’s not without its complications. What some are hailing as a miracle, others may see as a temporary fix that skirts the real work of developing healthier habits for long-term health.
Ultimately, like most things in medicine, Ozempic isn’t a one-size-fits-all solution. It offers remarkable benefits for those who need it, but it also comes with its own set of risks and challenges. As we continue to navigate this new era of “quick-fix” weight loss drugs, it’s essential to consider both the potential and the limitations of this medication and to remember that lasting health involves more than just a prescription.